Republished from kffhealthnews.org
When Karla Adkins looked in the rear view mirror of her car one morning nearly 10 years ago, she noticed the whites of her eyes had turned yellow.
She was 36 at the time and working as a physician liaison for a hospital system on the South Carolina coast, where she helped build relationships among doctors. Privately, she had struggled with heavy drinking since her early 20s, long believing that alcohol helped calm her anxieties. She understood that the yellowing of her eyes was evidence of jaundice. Even so, the prospect of being diagnosed with alcohol-related liver disease wasn’t her first concern.
“Honestly, the No. 1 fear for me was someone telling me I could never drink again,” said Adkins, who lives in Pawleys Island, a coastal town about 30 miles south of Myrtle Beach.
But the drinking had caught up with her: Within 48 hours of that moment in front of the rearview mirror, she was hospitalized, facing liver failure. “It was super fast,” Adkins said.

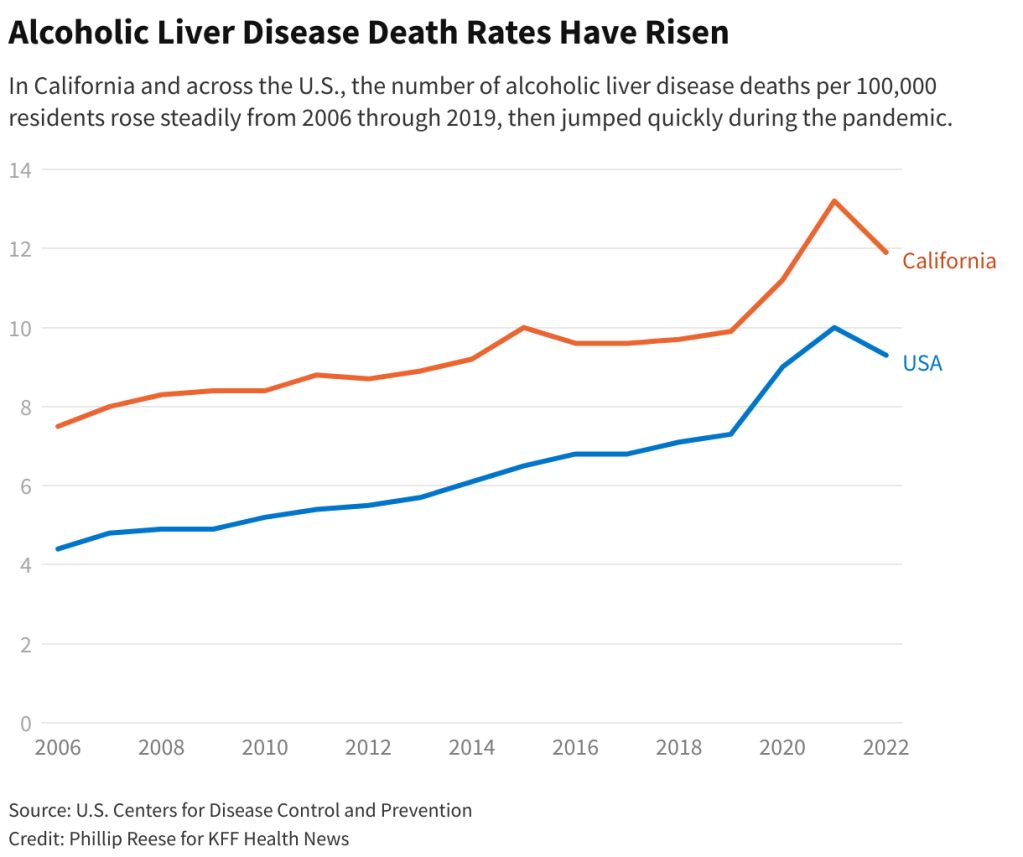
Historically, alcohol use disorder has disproportionately affected men. But recent data from the Centers for Disease Control and Prevention on deaths from excessive drinking shows that rates among women are climbing faster than they are among men. The Biden administration considers this trend alarming, with one new estimate predicting women will account for close to half of alcohol-associated liver disease costs in the U.S. by 2040, a $66 billion total price tag.
It’s a high-priority topic for the Department of Health and Human Services and the Department of Agriculture, which together will release updated national dietary guidelines next year. But with marketing for alcoholic beverages increasingly geared toward women, and social drinking already a huge part of American culture, change isn’t something everyone may be ready to raise a glass to.
“This is a touchy topic,” said Rachel Sayko Adams, a research associate professor at the Boston University School of Public Health. “There is no safe level of alcohol use,” she said. “That’s, like, new information that people didn’t want to know.”
Over the past 50 years, women have increasingly entered the workforce and delayed motherhood, which likely has contributed to the problem as women historically drank less when they became mothers.
“Parenthood tended to be this protective factor,” but that’s not always the case anymore, said Adams, who studies addiction.
More than 600,000 people in the U.S. died from causes related to alcohol from 1999 to 2020, according to research published in JAMA Network Open last year, positioning alcohol among the leading causes of preventable death in this country behind tobacco, poor diet and physical inactivity, and illegal drugs.
The World Health Organization and various studies have found that no amount of alcohol is safe for human health. Even light drinking has been linked to health concerns, like hypertension and coronary artery disease and an increased risk of breast and other cancers.
More recently, the covid-19 pandemic “significantly exacerbated” binge-drinking, said George Koob, director of the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health, as people used alcohol to cope with stress. That is particularly true of women, who are more likely to drink alcohol because of stress than men, he said.
But women are also frequently the focus of gender-targeted advertising for alcoholic beverages. The growth of rosé sales and low-calorie wines, for example, has exploded in recent years. New research published by the International Journal of Drug Policy in February found that the “pinking of products is a tactic commonly used by the alcohol industry to target the female market.”
Also at play is the emergence of a phenomenon largely perpetuated by women on social media that makes light of drinking to deal with the difficulties of motherhood. The misperception of “mommy wine culture,” said Adams, is that “if you can drink in a normal way, a moderate way, if you can handle your alcohol, you’re fine.”
And while it’s unclear to what extent memes and online videos influence women’s drinking habits, the topic merits further study, said Adams, who with colleagues last year found that women without children at age 35 are still at the highest risk for binge-drinking and alcohol use disorder symptoms among all age groups of women. But over the past two decades, the research concluded, the risk is escalating for both childless women and mothers.
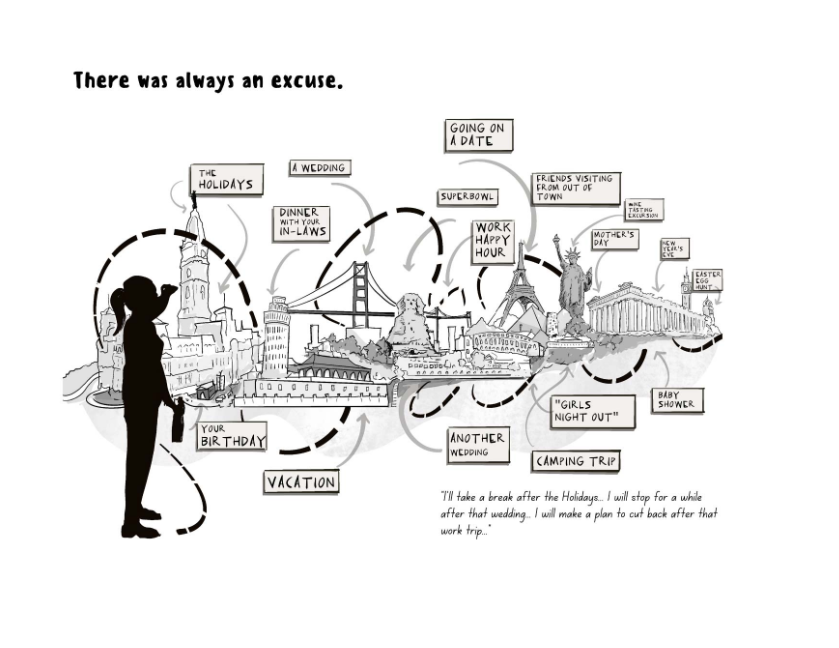
These factors at play, coupled with the pressure to fit in, can make excessive drinking a difficult conversation to broach.“It’s a very taboo topic,” Adams said.
And when it does come up, said Stephanie Garbarino, a transplant hepatologist at Duke Health, it’s often surprising how many patients are unaware how their drinking affects their health.
“Often, they didn’t know there was anything wrong with what they’re doing,” she said. She is more frequently seeing younger patients with liver disease, including men and women in their 20s and 30s.
And public health and addiction experts fear that alcohol-related liver disease among women will become a costly issue for the nation to address. Women accounted for 29% of all costs associated with the disease in the U.S. in 2022 and are expected to account for 43% by 2040, estimated a new analysis published in the American Journal of Gastroenterology in February.
National dietary guidelines advise women to drink no more than one alcoholic drink a day. Those guidelines are up for a five-year review next year by the USDA and HHS, which has called a special committee to examine, among other questions, the relationship between alcohol consumption and cancer risks. The report will be made public in 2025.
When Canada published guidance in 2023 advising that drinking any more than two alcoholic beverages a week carried health risks, Koob sparked backlash when his comments to the Daily Mail suggested that U.S. guidelines might move in the same direction. The CDC report published in February suggested that an increase in alcohol taxes could help reduce excessive alcohol use and deaths. Koob’s office would not comment on such policies.
It’s a topic close to Adkins’ heart. She now works as a coach to help others — mostly women — stop drinking, and said the pandemic prompted her to publish a book about her near-death experience from liver failure. And while Adkins lives with cirrhosis, this September will mark 10 years since her last drink.
“The amazing thing is, you can’t get much worse from where I got,” said Adkins. “My hope is really to change the narrative.”


You must be logged in to post a comment.