I’d thought long and hard about what I wanted to do when Will — and, soon after, his brother, Theo — returned home. The by-the-book Dr. Anthony Fauci approach would have been to have the boys keep on their masks, send them upstairs for a couple of weeks, and open all the windows in the house in the meantime.
But as the pandemic has taught us, there are things we value more than perfect protection from the virus. When it comes to them, we’re willing to puncture our bubbles, because without them, living feels like something less than being fully alive…
I admit that, at least to an outsider, my behavior seems inconsistent. But to me, it makes perfect sense. The risks I’m choosing to take are the ones where the payoff is biggest relative to the risk I perceive. (Yes, even the haircut! I love a good high-and-tight, and my barber is applying the clippers in his open-air home workshop.)
Before you argue with me, I get it. These aren’t the choices you would make. And that’s my point.We all have things we value. And risks we are willing to take for them. Neither of these two categories will be exactly the same for any one of us.
When it comes to the virus, we are all consistently inconsistent
Adam Cohen Published: Sun, December 13, 2020 1:07 AM Updated: Sun, December 13, 2020 1:36 AM — https://oklahoman.com/article/5678132/cohen-when-it-comes-to-the-virus-we-are-all-consistently-inconsistent
Exposed to grandchildren? Why take the chance?
reader comment
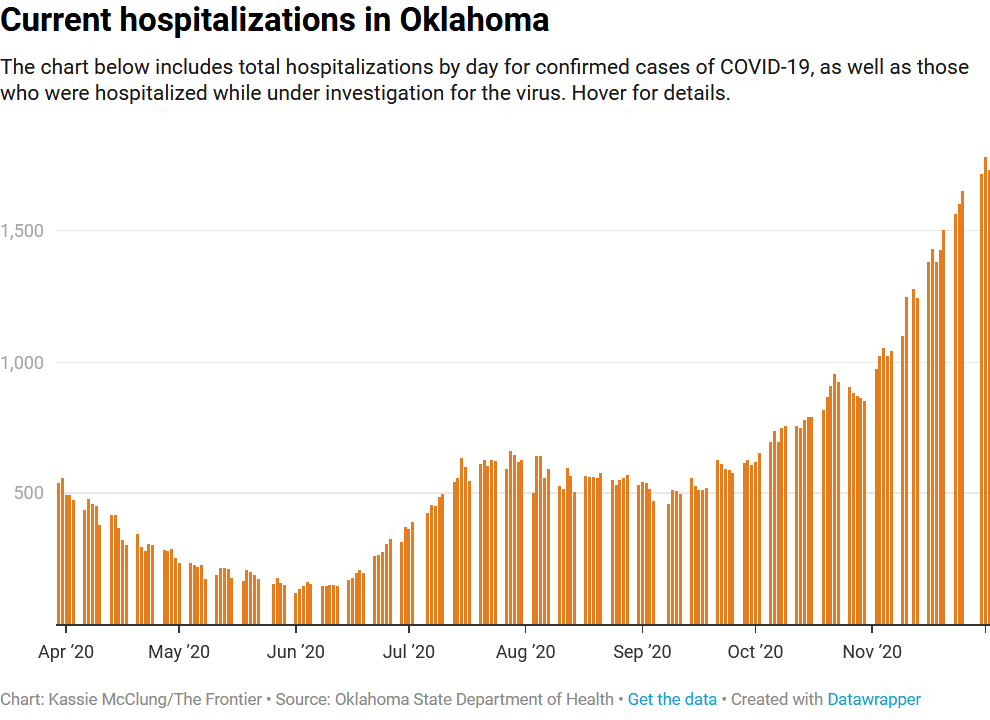
A reader’s comment above stopped me in my tracks. The past nine months have been spent mostly in the house with minimal forays out of the house for essentials like food and beer. I didn’t get a real haircut for months. The insides of a restaurant are now foreign to me. I cancelled my gym membership. So the comment made me think, why did I take the chance to spend time with Tiny Human Petri Dishes? When I stumbled upon the Cohen article I realized I was not alone. Nine months have disappeared and we all struggle with our own individual risk/reward scenarios.
The Grandchildren Bubble is unique. Risk was reduced to zero for six months. After six months all of the adults decided the Covid risk was minimal for several reasons. Two of the four adults (the most cautious and conservative ones) caught the virus. Thankfully both were fairly mild cases on the spectrum of asymptomatic to death and both have fully recovered. So two people have antibodies. The third adult is a front line HCW who deals with Covid each and every time he goes to work. The doctor has gotten tested multiple times all with negative results. One Tiny Human attends preschool and if a child has anything near a small sniffle they have to stay home and cannot rejoin the class until they have a negative Covid test. She recently received a negative test. Tiny Human Too just started crawling and doesn’t get out the house much. Not much to worry about here.
And for readers who have been counting that leaves yours truly. I lived with one of the infected before we knew she was infected. I tested negative the day before she got her test results. One of our neighbors asked if I left the house to live in a hotel. No I didn’t. Living apart while under the same roof was an interesting experience that I hope never to repeat. And despite having Covid in the house I didn’t catch it.
So I spent some time in my only trusted bubble mask less and I end up catching one or two non-Covid-19 coronaviruses. Next time I’m wearing a mask.


You must be logged in to post a comment.